Managing regulatory compliance across the entire product lifecycle has never been more complex or critical as medical devices become increasingly software-driven and connected. For a medical device, the path from concept to commercialization is a continuous loop of development, approval, monitoring, and improvement — all under the watchful eye of regulatory bodies worldwide. OEMs, whether introducing a new device to market or maintaining a fleet of existing connected products, must understand and implement a strategy to manage devices throughout the product lifecycle. It is essential for survival in today’s regulatory landscape.
Both the FDA and the EU MDR now share a lifecycle-centric philosophy to medical device safety and, therefore, regulation. Rather than treating market approval as the finish line, both frameworks require continuous oversight from initial concept through post-market surveillance and eventual retirement.
For the FDA, the concept of integrating premarket and post-market regulatory activities across a product's lifecycle began in the early 2000s, with a formal focus on lifecycle-driven compliance implemented in 2023.
The EU followed a similar trajectory. The MDR replaced the previous Medical Device Directive (MDD), often criticized for its passive and reactive approach to post-market monitoring. The MDR now mandates proactive and systematic surveillance throughout a device's lifetime, requiring manufacturers to continuously collect, analyze, and act on real-world performance data.
Both regulations evolved towards a lifecycle approach, with the understanding that manufacturers must actively maintain device safety throughout a product's entire existence.
The US FDA's Total Product Lifecycle Approach
The US Food and Drug Administration (FDA) takes a Total Product Lifecycle (TPLC) approach to regulating medical devices. Rather than simply focusing on market approval, the TPLC model emphasizes continuous oversight from the moment a device is conceived to final decommissioning. The TPLC approach consists of three phases: pre-market development, market approval, and post-market activities.
During pre-market development, manufacturers must establish rigorous design controls, implement comprehensive risk management strategies, and complete thorough verification and validation considerations. The goal is to integrate safety and effectiveness into the device from the outset, focusing on future-proofing and patient safety from the beginning.
Market approval follows, requiring complete and compliant documentation. Manufacturers submit this documentation through the appropriate pathway, including 510(k) pre-market, De Novo, or Pre-market approval (PMA). However, the approval process is just the beginning of releasing and monitoring a compliant medical device.
Post-market activities demand ongoing surveillance, systematic complaint handling, and structured change control to monitor real-world performance, address emerging issues, and ensure continued compliance throughout the device's commercial life.
The EU MDR's lifecycle and quality framework
Building upon the preceding MDD-93/42 ECC regulation, the European Union's Medical Device Regulation (MDR) adopts a complementary approach to medical device management with a greater focus on the development and design process. The MDR framework centers on lifecycle and quality management, with particular emphasis on patient safety and proactive, patient-centric risk mitigation. It requires OEMs to clearly define a device's intended purpose, conduct comprehensive risk assessments, and gather clinical evidence that genuinely supports claims of safety and performance in real-life applications and edge cases.
Furthermore, the MDR mandates extensive documentation and traceability requirements; manufacturers must maintain detailed technical files, ensure full traceability of all device components, and apply rigorous risk management to materials and manufacturing processes. The MDR also requires a Quality Management System (QMS) aligned with ISO 13485:2016, covering all aspects of device realization, production, and service provision.
Most significantly, the MDR places heavy emphasis on ongoing clinical evaluation and post-market surveillance. Real-world evidence is a continuous requirement, shaping how manufacturers monitor, update, and improve devices throughout their commercial lives.
Lifecycle considerations across FDA regulations and the MDR
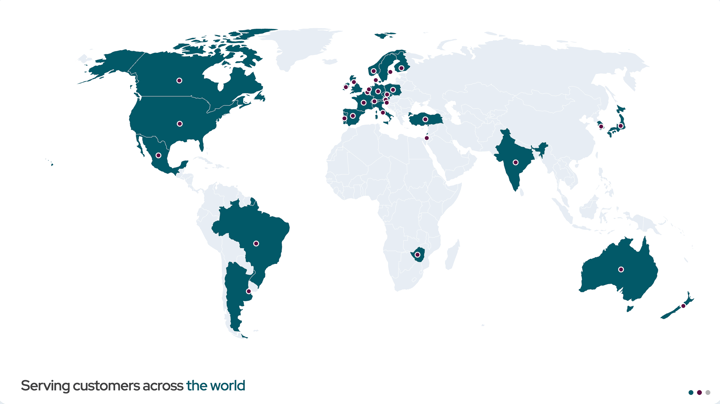
Medical device requirements – both those in the US, governed by the FDA, and in the EU, governed by the MDR – require ongoing maintenance, consideration, and overall surveillance throughout the device’s lifecycle to promote patient safety and device success. The compliance requirements differ across global legislations, but there is an overlap in the lifecycle considerations required in device development and ultimately circulation through the market.
Phase 1: Concept and feasibility
At the beginning of every device lifecycle, both frameworks require you to define the objective of the device. The FDA refers to this as "intended use," while the MDR refers to "intended purpose." And each framework requires a risk-based classification. The MDR applies specific rules, such as Rule 11 for software classification, whereas the FDA uses Product Codes and regulatory pathways, including the 510(k) and PMA routes.
Phase 2: Design and development
The design and development phase requires robust design controls, risk management aligned with ISO 14971, and software lifecycle processes that follow IEC 62304. The MDR emphasizes demonstrating conformity with General Safety and Performance Requirements (GSPR) and conducting early clinical evaluation. The FDA guidelines focus on Design History Files (DHF) and tracing user needs through design inputs.
For embedded software, lifecycle documentation is particularly critical, with requirements to:
- maintain the version history of firmware and software builds,
- complete change impact assessments and risk re-evaluations,
- develop traceability matrices that link requirements to code to tests, and
- archive configurations for each market release.
Under the FDA, the DHF and Device Master Record (DMR) include this information, while the MDR requires a detailed technical file with GSPR mapping.
Phase 3: Verification and validation
In Phase Three, manufacturers must demonstrate that their device meets the specified requirements and is genuinely safe and effective. Phase Three includes usability engineering in accordance with IEC 62366, cybersecurity validation, and comprehensive software and system verification and validation (V&V) activities. The MDR requires particularly detailed documentation of clinical benefits and safety for higher-risk devices.
Phase 4: Submission and approval
Formal regulatory submission is the last step in pre-market approvals, which includes: a 510(k), De Novo, or PMA for the FDA, or technical documentation for MDR review. The key difference at this phase is that the FDA grants approvals directly, while MDR approval for all but the lowest-risk devices requires involvement of a Notified Body. Both systems require the assignment of Unique Device Identification (UDI) and compliance with regulatory labeling requirements.
Phase 5: Production and distribution
Once manufacturing begins, both FDA regulations and the MDR require certified Quality Management Systems. The FDA enforces this through 21 CFR Part 820, while MDR Chapter VII typically requires compliance with ISO 13485. Both regulations mandate proper labeling, traceability, and complaint handling systems. The MDR adds an additional requirement to register in the EUDAMED database.
Phase 6: Post-Market surveillance
Both regulations emphasize post-market surveillance and require a large amount of ongoing commitment and focus from OEMs. The FDA mandates Medical Device Reporting under 21 CFR Part 803, device corrections and removals (recalls) under 21 CFR Part 806, and corrective and preventative actions (CAPA) processes under 21 CFR Part 820.100. The MDR emphasizes the importance of continuous evaluation through Post-Market Surveillance (Articles 83–86), Post-Market Clinical Follow-up (Article 74), and Periodic Safety Update Reports (Article 86).
For embedded software, configuration management becomes critical during post-market surveillance. Regulators expect clear answers to questions. Which firmware version is currently deployed in the field? What dependencies and third-party components are involved in this device? How is traceability maintained from source code to binary? Real-world performance monitoring — including analytics, telemetry, cybersecurity threat detection, and user-reported issues — must also be integrated into device surveillance systems.
Building a compliance-ready organization
Building organizational capabilities that make compliance sustainable is the key to excelling with regulations from the FDA and the MDR. First, develop a comprehensive lifecycle management strategy that outlines procedures for every stage, from design to post-market. The strategy should be clearly communicated throughout the organization so that everyone understands their role in maintaining compliance.
Second, implement a robust QMS that encompasses documentation, risk management, and continuous improvement — including CAPA processes, complaint handling, and vigilance reporting. The QMS should be flexible enough to accommodate both FDA and MDR requirements without creating parallel systems that drain resources.
Third, leverage digital tools for documentation, change management, and real-time monitoring. Modern software platforms can dramatically improve transparency and streamline compliance responsibilities when properly implemented and integrated with existing workflows.
Fourth, conduct regular audits of device inventory and compliance processes, and provide ongoing training to maintain regulatory awareness across the team. Compliance requires continuous attention and investment.
Finally, plan proactively for regulatory changes. The global regulatory landscape continues to evolve, and manufacturers who wait until changes are mandatory often find themselves scrambling to catch up. Building regulatory intelligence into the planning processes helps avoid costly delays and non-compliance situations.
Ongoing compliance as regulations adapt
The key to understanding the complexity of regulations from the FDA and the MDR is recognizing that compliance is an ongoing commitment that begins at concept and continues through decommissioning.
By investing in robust documentation systems, building quality into development processes, and treating post-market surveillance as a source of valuable insights rather than a regulatory burden, manufacturers can transform compliance from an obstacle into a competitive advantage.
New guidance documents will emerge, standards will be updated, and expectations will shift. But, manufacturers who build adaptable systems, grounded in the fundamental principles of safety, effectiveness, and quality, will be well-positioned to meet whatever challenges come next.
Recent articles
New Mender experimental AI-enabled feature
Mender in 2025: A year in review with compliance, security, and AI-driven growth
What’s new in Mender: Enhanced delta updates and user experience
Learn why leading companies choose Mender
Discover how Mender empowers both you and your customers with secure and reliable over-the-air updates for IoT devices. Focus on your product, and benefit from specialized OTA expertise and best practices.