The critical role that security and safety requirements play in software-driven medical devices
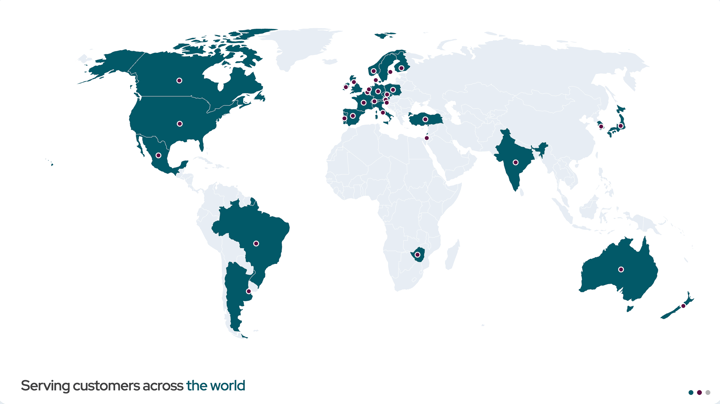
Largely due to the growth of IoT and AI/ML, medical devices have become increasingly software-driven and interconnected over the past decade. Innovative technology brings opportunities to redefine the medical device and healthcare industries: from simple health-focused wearables to sophisticated AI-powered diagnostic systems. Cloud connectivity, remote patient monitoring, and real-time data analytics are now standard features in smart medical devices rather than competitive differentiators.
Embracing connectivity in medical devices enables unprecedented clinical capabilities; devices can learn from population-level data, receive over-the-air updates to improve performance, and integrate seamlessly into electronic health records (EHR). However, this interconnectedness also introduces new vectors for cybersecurity threats, requires continuous software maintenance, and creates complex regulatory obligations that extend far beyond traditional medical devices. Historically, the medical industry manages data governance and privacy on a more severe level and scale than other industries; and, as the prominence of connected technologies increases operational complexity, regulatory frameworks must evolve to match this heightened complexity.
Manufacturers face a complex regulatory landscape that demands both innovation and rigorous compliance to adapt and compete in a rapidly changing industry.
Navigating emerging requirements
Navigating emerging requirements is essential to offer safe, effective medical devices while maintaining a competitive advantage in the global healthcare ecosystem. Manufacturers who build robust quality systems and demonstrate regulatory excellence gain faster market access, reduce costly delays from non-conformities, and build trust with healthcare providers and patients. Proactive compliance becomes required in an industry where time-to-market determines market leadership and recall costs are devastating. OEMs must design devices with security, ongoing maintenance, and compliance in mind from the onset. Compliance is a strategic differentiator in the connected healthcare space.
The regulatory landscape itself demands innovation–from OEMs and the frameworks themselves–because static, one-time products and approval processes are insufficient for software-driven devices that continuously evolve. Regulators increasingly expect manufacturers to demonstrate both initial safety and efficacy, as well as ongoing capabilities to manage updates, monitor post-market performance, and respond rapidly to emerging risks — across multiple international jurisdictions.
Compliance with the US FDA and the EU MDR
The US FDA and EU MDR are regulatory frameworks for medical devices. Both focus on safety, efficacy, and quality, but differ in scope and implementation. The US FDA oversees the medical devices in the US market through premarket approval, risk classification, and post-market surveillance. The EU MDR, enforceable across the European Union, is stricter than the previous Medical Device Directive and emphasizes clinical evaluation, unique device identification, and post-market monitoring.
These two regulations cover the entire device lifecycle, placing more responsibility on manufacturers, especially for software-driven and high-risk devices. At a high level, the US FDA and EU MDR regulations focus on the safety and security of medical technology for patient care. Despite different jurisdictions, many similarities exist between the two regulations that allow OEMs to standardize on best practices that achieve global compliance.
Both the US FDA and EU MDR stand to assess device compliance before market availability. The FDA has two assessment pathways: 1) 510(k) for moderate risk, where manufacturers must demonstrate substantial equivalence to an existing device, and which the FDA reviews without third-party involvement, and 2) pre-market approval for high-risk devices.
The MDR involves a more rigorous assessment and documentation across all risk levels. Understanding both frameworks is crucial for achieving global market access and maintaining long-term compliance.Between the two regulations, various differences exist that must also be considered when determining the best course of action to achieve compliance and success in the medical device industry. The complexity of dual compliance stems from the fact that, while both frameworks share common goals around patient safety and device effectiveness, they differ in their procedural requirements and documentation standards. The differences create challenges and opportunities for manufacturers seeking to operate across international markets.
Medical device manufacturers face many compliance challenges under the US FDA and EU MDR, especially around embedded software updates and device lifecycle management (DLM). Key regulatory challenges include:
- Maintaining compliance without compromising device cybersecurity or clinical performance
- Ensuring all software changes, updates, or patches are documented and traceable.
Quality system processes must support change control and link to unique device identification, post-market surveillance, and corrective and preventive action activities.
For software-driven devices, compliance is an ongoing process; each update or modification can present regulatory challenges for manufacturers. The rapid pace of software innovation makes navigating regulations more complex. Proactively addressing these challenges enhances quality, improves reliability and safety, and adds value for both patients and healthcare providers.
The scale and stakes of medical device safety
The growth of connected medical devices creates enormous responsibility for OEMs. In the US alone, over 10% of the population (around 35 million people) has a medical device implanted. By 2034, the implantable medical device market is expected to reach a valuation of $176.33 billion globally. The scale of medical devices underscores the importance of evolving regulatory frameworks alongside technology. Medical devices are not as simple as consumer electronics, which can be replaced if they malfunction; medical devices sustain life, restore function, and directly impact patient well-being.
The stakes of a malfunction become clear when examining the data. According to the US FDA, more than 80,000 deaths and 1.7 million injuries in the past decade are linked to medical devices. The side effects of loose regulation materialize in real human consequences. Consider the case of faulty metal-on-metal hip replacements that left patients with permanently destroyed muscles, tendons, and essential organs. This is far from an isolated incident; medical device failures carry profound consequences. When a pacemaker fails, when an insulin pump malfunctions, when a surgical robot experiences a software error, lives hang in the balance.
Some critics argue that stringent regulatory requirements stifle innovation, create barriers to entry for smaller manufacturers, and slow the pace at which beneficial technologies reach patients. There's merit to concerns about regulatory efficiency, and both the FDA and MDR have implemented pathways to accelerate approval for breakthrough devices. However, the argument that regulations fundamentally impede progress misses a crucial point: robust regulatory frameworks enable sustainable innovation while protecting key stakeholders throughout the process. The fundamental focus in medical and healthcare technology must be the well-being of the patient. And regulations, at a very high level, act to ensure this remains constant throughout product development and deployment.
Regulation as a foundation of trust
Without rigorous oversight, the medical device and healthcare industry would face a crisis of confidence. Healthcare providers would hesitate to adopt new technologies without assurance of safety and efficacy. Insurance reimbursement would become unpredictable. Most critically, patient harm would increase, leading to litigation, recalls, and market instability, ultimately costing manufacturers far more than compliance investments. The regulatory process, when properly implemented, serves as quality assurance that protects both patients and manufacturers' long-term viability.
Not to mention, connected devices introduce unprecedented complexity. A traditional mechanical heart valve, once implanted, performs a fixed function. A software-driven cardiac monitoring device, by contrast, may receive dozens of updates over its lifecycle, communicate with multiple systems, and process sensitive patient data vulnerable to cyberattacks. The regulatory challenge isn't whether to innovate, it's how to innovate responsibly in today’s environment–where software updates can be deployed to thousands of patients simultaneously, a single cybersecurity vulnerability could compromise an entire device class, or post-market surveillance must catch unintended consequences.
Understanding both US FDA and EU MDR requirements is essential; manufacturers must build compliance into their development processes from day one, treating regulatory strategy as a core competency rather than an afterthought.
Between these regulatory touchpoints lies the critical work of ongoing device management. Software updates, security patches, and feature enhancements must all be carefully controlled and documented. The middle ground, where innovation meets regulation, is where manufacturers must build robust processes that support both agility and compliance. The stakes are particularly high for connected devices, where cybersecurity vulnerabilities can emerge rapidly and require swift response while maintaining regulatory compliance.
For manufacturers, success depends on establishing quality management systems that accommodate the dynamic nature of software while satisfying the static requirements of regulatory documentation. This means OEMs must track and document every software change—not as a checkbox exercise, but because undocumented modifications can introduce defects that go undetected until after market release. When a manufacturer updates a diagnostic algorithm, they need records showing what changed, why, and what testing validated it. This traceability is the difference between quickly identifying the root cause of a field issue versus spending months investigating.
Post-market surveillance must feed directly back to engineering teams. When hospitals report unexpected device behavior, engineers need a clear path to investigate and implement fixes. Software updates to patch security vulnerabilities follow the same principle; they're essential responses to real threats, not optional maintenance.
The central challenge facing medical device manufacturers today is maintaining compliance throughout a device's entire operational life. As software becomes the primary mechanism through which devices evolve, improve, and respond to emerging threats, the update process itself becomes a critical competency. Software updates in modern medical devices are the backbone of ongoing compliance, acting as routine operations that must be executed with precision and full regulatory awareness.
Every update carries the potential to improve patient outcomes, while similarly introducing risk if not properly validated and documented. A key component of innovation today revolves around how to distribute updates and security patches in a manner that satisfies regulatory obligations, maintains device safety, protects against cybersecurity threats, and delivers clinical value.
Ensuring safe and innovative healthcare through software updates
In today's interconnected healthcare environment, software updates are essential drivers of innovation. Whether for diagnostics, monitoring, or therapy delivery, updates are crucial for improving patient outcomes, integrating new clinical insights, and maintaining a device's competitive advantage.
However, software updates involve regulatory, safety, and cybersecurity risks. Managing updates requires a structured, well-documented process that aligns with international standards and regulatory expectations.
Manufacturers must adapt the overall product development strategy to provide the best patient-centric experience. Regulatory controls and secure design must be embedded into the core product strategy and evolve alongside the development lifecycle with heightened cybersecurity measures.
A disciplined update process goes hand in hand with a robust, lifecycle-focused compliance strategy. Overall, supporting regulatory compliance with ongoing updates builds market trust, reduces liability, and positions manufacturers to lead in a rapidly evolving digital health ecosystem.
Recent articles
New Mender experimental AI-enabled feature
Mender in 2025: A year in review with compliance, security, and AI-driven growth
What’s new in Mender: Enhanced delta updates and user experience
Learn why leading companies choose Mender
Discover how Mender empowers both you and your customers with secure and reliable over-the-air updates for IoT devices. Focus on your product, and benefit from specialized OTA expertise and best practices.