The differences between the US FDA’s device approval process and the EU’s medical device regulation (MDR): An essential dual-compliance framework for global manufacturers
Releasing connected products into the global marketplace requires a vigorous understanding and application of security and regulatory standards. To ensure compliance and user protection, the medical industry enforces some of the strongest regulations due to the life-critical nature of product uses and the possible severity of consequences resulting from device failure. The intersection of these regulations and connected medical devices allows advancements in the healthcare world to embrace endless innovation while requiring increased regulatory oversight.
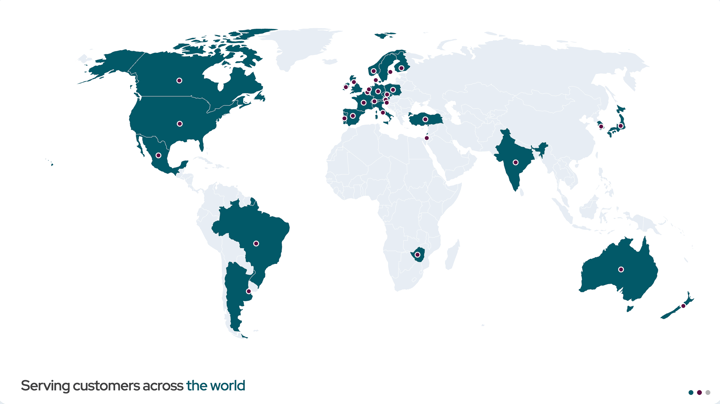
Today, global medical device manufacturers face a formidable challenge: navigating two of the world's most influential regulatory frameworks simultaneously. The U.S. Food and Drug Administration (FDA)’s approval process for medical devices and the European Union's Medical Device Regulation (MDR) both aim to protect patient safety. However, each approaches this goal with distinctly different philosophies and requirements.
For manufacturers seeking global market access, understanding the differences between the two approval approaches is essential for launching a compliant product that protects patients and improves care outcomes.
Why both medical device frameworks matter
The frameworks from the US FDA and the European Union’s MDR share a fundamental mission: ensuring medical devices are safe, effective, and of high quality. However, their paths to achieving this goal diverge in scope, process, and documentation expectations. The FDA has long served as the gatekeeper for the U.S. market, employing risk-based classification and premarket review processes that evolved over decades. Meanwhile, the European Union recently adopted the MDR, which entered force in 2017 and replaced the previous Medical Device Directive with far more rigorous requirements.
For connected devices, these regulatory differences become especially pronounced. Connected medical devices that receive over-the-air (OTA) updates, process sensitive patient data, and integrate with electronic health records (EHR) systems must satisfy both frameworks' evolving expectations around cybersecurity, post-market surveillance, and lifecycle management. The challenge extends beyond creating novel technology. Medical device OEMs must build products that meet the highest standards of both markets while maintaining the agility to innovate.
The EU MDR approach: Comprehensive and lifecycle-focused
The EU MDR adopts a prescriptive, lifecycle-oriented approach to regulating medical devices. Under this framework, conformity assessment processes scale with the risk of the device. Low-risk Class I devices can undergo manufacturer self-assessment; as risk increases through Classes IIa, IIb, and III, oversight intensifies correspondingly. Higher-risk devices require certification from a Notified Body — an authorized third-party organization that evaluates technical documentation, clinical data, and regulatory compliance before any device can reach the market.
The MDR differs in its emphasis on comprehensive documentation and continuous oversight. The regulation requires extensive technical files that demonstrate compliance with the General Safety and Performance Requirements (GSPR). While similar in concept to the US FDA's design controls, the MDR necessitates more detailed specifications for software validation and clinical evidence. Every aspect of the device lifecycle must be documented, from initial design through post-market performance.
Post-market surveillance under the MDR is mandatory and systematic. Manufacturers must establish robust systems for monitoring device performance, promptly reporting incidents, and implementing safety corrective actions in the field when issues arise. The Unique Device Identification (UDI) system ensures complete traceability across production, deployment, and field operations, with software versions explicitly tracked.
The European Database on Medical Devices (EUDAMED) serves as a central transparency and tracking system. Guidance from the Medical Device Coordination Group (MDCG) provides crucial clarifications on clinical evaluation, software qualification, cybersecurity, and other critical areas. Documents from these entities inform the MDR framework, effectively serving as best practices for manufacturers preparing regulatory submissions.
The US FDA framework: Risk-based and pathway-driven
The US FDA's regulatory approach centers on risk classification and establishing appropriate review pathways. Devices fall into three classes based on their risk profile, with Class III representing the highest risk category. The pathway a device takes to market depends primarily on 1) this classification and 2) whether substantial equivalence to an existing device in the market can be demonstrated.
For moderate-risk Class II devices, the 510(k) notification process serves as the primary pathway for market approval. For 510(k) market approval, manufacturers must demonstrate that their device is substantially equivalent to a legally marketed predicate device. This pathway emphasizes comparative analysis rather than absolute clinical proof, making it faster and less resource-intensive than alternatives. However, if no suitable predicate device exists, manufacturers must either pursue device reclassification with supporting evidence or proceed through the more rigorous Premarket Approval (PMA) process.
Required for high-risk Class III devices and moderate-risk Class II devices without a predicate device, the PMA pathway demands extensive evidence, including clinical trial data to demonstrate safety and effectiveness. The PMA process involves a thorough scientific review and represents the US FDA's most stringent evaluation mechanism.
The FDA's Quality System Regulation (21 CFR Part 820) establishes essential quality management requirements, including design controls, verification and validation procedures, and change management processes. For software-driven devices, 21 CFR Part 11 imposes specific requirements regarding electronic records and signatures and ensuring digital traceability throughout development and manufacturing.
The US FDA guidance documents on Software as a Medical Device (SaMD), software modifications, cybersecurity, and AI/ML-based software provide critical direction for manufacturers navigating the increasingly software-centric medical device landscape.
Achieving compliance: Key differences that matter in practice
While both frameworks aim to promote patient safety through risk-based oversight, their practical implementation differs in ways that significantly impact manufacturers' operations.
Documentation expectations represent a major divergence. The EU MDR prescribes structured documentation requirements through Annexes II and III, leaving less room for interpretation. The US FDA's approach, while comprehensive, allows more flexibility in how manufacturers present their evidence, which can lead to variability in submission content and quality.
Clinical evidence requirements also differ substantially between the two frameworks. The EU MDR mandates continuous clinical evaluation throughout a device's lifecycle, with specific requirements outlined in Annex XIV. The US FDA clinical evidence requirements vary by approval pathway; the PMA process requires extensive clinical data, while the 510(k) application may rely more heavily on comparative analysis and bench testing.
Post-market surveillance obligations are explicit and detailed under the MDR, with clear specifications for content, timing, integration, and responsibilities outlined in Annex III and Articles 83-86. The US FDA requirements under 21 CFR Parts 803 and 822 are less prescriptive, though no less important in practice.
Organizational requirements in the EU MDR require manufacturers to designate a Person Responsible for Regulatory Compliance (PRRC) — a specific role with defined responsibilities. The US FDA requires quality management personnel, but doesn't mandate the details of the particular position(s).
Perhaps most fundamentally, the authorization process itself differs between the two frameworks. In Europe, manufacturers work with Notified Bodies for higher-risk devices and issue a Declaration of Conformity to achieve the CE Marking. In the US, the FDA acts as the centralized reviewer, granting Clearance (for 510(k)) or Approval (for PMA) directly.
Navigating dual compliance with the EU MDR and US FDA
The complexity of achieving compliance with both frameworks stems from their different procedural requirements and documentation standards, despite sharing common goals.
A Class III device under the MDR roughly corresponds to a Class III or novel (no predicate) Class II device that must achieve PMA by the FDA. MDR Class IIa and IIb devices generally align with moderate-risk Class II devices gaining approval through the FDA 510(k) process. However, device classification under both frameworks is nuanced, and manufacturers must carefully map their specific device characteristics to each framework's requirements for proper classification.
Quality system expectations are also a challenge. The MDR references ISO 13485:2016 through its conformity assessment annexes. The US FDA currently refers to 21 CFR Part 820 as its Quality System Regulation. However, the US FDA will align more closely with ISO 13485 through its Quality Management System Regulation (QMSR), effective February 2026. Historically, manufacturers navigated two distinct quality system frameworks, but these may more closely align in the near future.
In addition to device classification, software classification presents another area requiring careful attention. The MDR applies Rule 11 from Annex VIII to classify software, while the FDA uses its own risk-based approach supported by digital health guidance documents. Manufacturers must ensure their software classification rationale satisfies the logic of both frameworks.
Building for better patient outcomes globally
Manufacturers seeking to operate in the US and EU markets face genuine challenges, but also significant opportunities. The key is treating regulatory strategy as a core competency from day one, not as an afterthought to product development.
Successful global manufacturers must:
- Develop quality management systems that meet the expectations of both frameworks while supporting innovation and agility.
- Establish processes for comprehensive documentation that meet the MDR's structured requirements while remaining flexible enough to support the US FDA approval submissions.
- Implement robust post-market surveillance systems that exceed both frameworks' minimum requirements, treating device monitoring as an opportunity to gather valuable real-world evidence rather than merely checking regulatory boxes.
For software-driven devices, manufacturers must also:
- Establish change control processes that link every modification to appropriate documentation, validation activities, and risk assessments.
- Building cybersecurity considerations into design from the beginning, not as an afterthought.
- Creating traceability systems that can track not just physical components but software versions, updates, and configurations across a device's entire operational life.
The manufacturers who thrive in this environment recognize that regulatory excellence drives competitive advantage.
- Faster, more predictable market access.
- Reduced risk of costly delays from non-conformities.
- Enhanced trust with healthcare providers, patients, and regulators.
- Lower likelihood of recalls and field actions.
The benefits of regulatory excellence far outweigh the investment in robust regulatory processes.
Building and maintaining compliance-ready devices
As medical devices become increasingly interconnected and software-driven, regulatory frameworks will continue evolving to address emerging risks and opportunities. Manufacturers who understand both the US FDA approval processes and the EU MDR — their similarities, differences, and changing requirements — position themselves to lead in the global healthcare ecosystem.
Making a strategic investment in compliance remains one of the key differentiators of leaders in the connected medical device space. By building quality and regulatory excellence into product development from the start, manufacturers create sustainable competitive advantages that enable innovation while protecting the patients who depend on their devices.
Recent articles
New Mender experimental AI-enabled feature
Mender in 2025: A year in review with compliance, security, and AI-driven growth
What’s new in Mender: Enhanced delta updates and user experience
Learn why leading companies choose Mender
Discover how Mender empowers both you and your customers with secure and reliable over-the-air updates for IoT devices. Focus on your product, and benefit from specialized OTA expertise and best practices.